Diseases
Kératitis

Definition
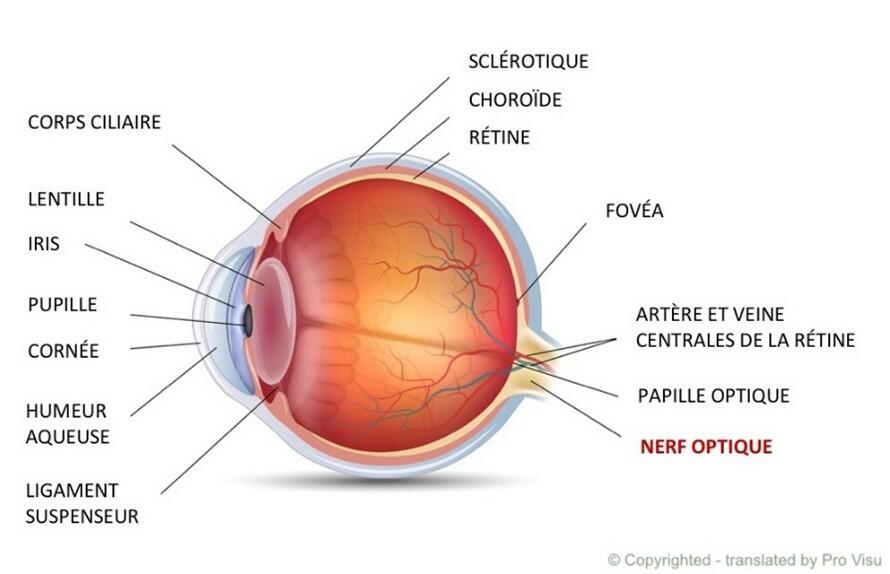
Keratitis is an inflammation of the first layer of the cornea, called the epithelium, which can cause severe pain due to its extensive innervation. Most often unilateral, keratitis can also affect both eyes and be associated with inflammation of the conjunctiva. It requires an ophthalmological consultation.
There are several types of keratitis:
- Bacterial keratitis: this type of keratitis is the most common, but must be treated to avoid the serious complication of corneal perforation.
- Herpetic keratitis: the herpes simplex virus is responsible for this infection, which often recurs and can even affect the deeper layers of the cornea and the iris. There are three types of herpes simplex keratitis (classified in order of severity): epithelial, disciform and stromal. Medical follow-up is necessary, as recurrences can result in ulceration, opacification, scar opacity, thinning of the corneal stroma and reduced vision.
- Viral keratitis: this is most often caused by herpes simplex, but adenoviruses can also cause viral keratitis, known as kerato-conjunctivitis, when inflammation of the cornea is added to that of the conjunctiva.
- Amebic keratitis: rare, this type of keratitis is caused by free-living amoebae and most often appears in contact lens wearers, although it can also occur in non-wearers, particularly after ocular trauma or exposure to contaminated water. A painful ulceration develops on the cornea and can impair vision. Medical follow-up is therefore necessary to make a rapid diagnosis and introduce treatment as early as possible.
- Traumatic keratitis: this is very painful and is mainly caused by a foreign body, fingernail or chemical being thrown into the eye, or by a burn to the corneal epithelium.
Toxic keratitis: often caused by the incorrect use of certain eye drops. - Snow keratitis: Also known as photokeratitis, this type of keratitis occurs after the eyes have been exposed to ultraviolet rays, particularly UVC, which burn the cornea and destroy the epithelium. This condition occurs when the sun's rays reverberate off snow (or water or sand to a lesser extent), and is akin to sunburn on the eye.
Causes
The causes depend on the type of keratitis and can be very diverse:
- Viral or bacterial infection
- Amoeba infection
- Poor hygiene of contact lenses
- Prolonged contact lens wear
- Dry eyes
- Ocular trauma
- Contact with chemicals
- Exposure to ultraviolet light
- A reaction to certain eye drops
- Blepharitis
Symptoms
There are several symptoms, although they may differ depending on the type of keratitis. The most common are pain, tearing, sensitivity to light, redness of the eyes and a sensation of a foreign body in the eye. Keratitis can also lead to vision problems.
Diagnosis
Diagnosis is based on a clinical examination of the symptoms and exposure to one of the known causes of the condition. Slit-lamp examination is also necessary, especially in the case of herpetic keratitis, where the presence of ulceration confirms the diagnosis.
In the case of suspected amoebic or bacterial keratitis, a sample taken from the cornea can be cultured to determine the pathogen responsible for the infection. If the patient wears contact lenses, these may also be analyzed.
Treatment
In the case of bacterial keratitis, a broad-spectrum antibiotic may be prescribed pending the results of the culture, which will then define a targeted antibiotic therapy. Ointments or eye drops may accompany the treatment to aid healing and relieve symptoms.
In the case of herpetic keratitis, most patients receive medical follow-up. This applies to epithelial and disciform keratitis, but is even more important in the case of stromal keratitis, which can lead to necrosis of the stroma and irreversible loss of vision. Antiviral treatment is prescribed, and corticosteroids may be combined with it for disciform or stromal keratitis (although they are contraindicated for epithelial keratitis).
Antimicrobial treatment (often in the form of eye drops) must be rapidly instituted for amebic keratitis. It lasts between 6 and 12 months, depending on healing, and should not be stopped too early to avoid the risk of recurrence. Sometimes, if antimicrobial treatment is insufficiently effective, or if the diagnosis is made too late, corneal repair surgery may be necessary.
In the case of snow keratitis, artificial tears reduce symptoms by lubricating the eye and promoting healing. A vitamin A-based ointment is also recommended to regenerate the epithelium. Finally, an antibiotic eye drop may be prescribed to prevent superinfection, which is potentially favored by corneal lesions.
Prevention
Generally speaking, good hand and contact lens hygiene helps limit the risk of keratitis. Always keep your hands clean when handling contact lenses. It's also important to remove them in the shower or in swimming pools and jacuzzis, to never clean them with water, to store contact lenses in the appropriate storage liquid, and to avoid abusing them for long periods. If you experience pain when wearing contact lenses, remove them promptly and consult an ophthalmologist.
Snow keratitis can be prevented by wearing sunglasses with appropriate filters (category 3 or higher) or a mask specifically designed for winter sports.
Keratitis is an inflammation of the first layer of the cornea, called the epithelium, which can cause severe pain due to its extensive innervation.
References
- https://www.hug.ch/sites/interhug/files/structures/medecine_de_premier_recours/documents/infos_soignants/oeil_rouge_arce.pdf
- https://www.daviel.fr/keratite/
- https://www.oeiletpaupiere.fr/chirurgie-reparatrice-de-lorbite-et-des-paupieres/le-trichiasis/
- https://www.msdmanuals.com/fr/professional/troubles-oculaires/troubles-corn%C3%A9ens/k%C3%A9ratite-herp%C3%A9tique?redirectid=3515?ruleredirectid=30
- https://www.areaoftalmologica.com/fr/corn%C3%A9e/k%C3%A9ratite/bact%C3%A9rien/
- https://www.msdmanuals.com/fr/accueil/infections/infections-parasitaires-protozoaires-extra-intestinaux/k%C3%A9ratite-amibienne-infection-oculaire
- https://blog.ophtalmique.ch/2022/12/06/keratite-des-neiges/#:~:text=Ses%20rayons%20ultraviolets%2C%20en%20particulier%20les%20UVC%2C%20sont,s%E2%80%99apparente%20%C3%A0%20un%20coup%20de%20soleil%20sur%20l%E2%80%99%C5%93il.
Content reviewed and controlled on 16.01.2025